1. Introduction
In recent years, Non-alcoholic Fatty Liver Disease (NAFLD) has received a lot of attention as the most common liver disease and one of the most important causes of chronic liver disease in children and adults [
1]. The main mechanism that leads to NAFLD is not fully known yet, but factors such as obesity, metabolic syndrome, lack of antioxidant resources in the body, genetics, unhealthy and sedentary lifestyle and poor nutrition can be effective in the development of this disease [
4]. Loquat is a subtropical plant belonging to the Rosaceae family with high medicinal value. It has been reported that the extracts of its various tissues (leaves, seeds and fruits) have great therapeutic effects in terms of biological activity. Ursolic acid has several biological activities including anti-oxidation, anti-inflammatory, anti-cancer and liver protection [
13]. On the other hand, exercise can have positive effects on the treatment, control and prevention of NAFLD. Exercise is one of the main regulators of hepatic metabolism by increasing beta oxidation and decreasing lipogenesis. Studies have shown that High Intensity Interval Training (HIIT) is a good strategy to reduce the plasma concentrations of liver enzymes, lipid profile, insulin resistance and fat content [
27]. This study aims to assess whether 8 weeks of HIIT with Loquat Leaf Extract (LLE) supplementation can affect the liver enzymes of obese men with NAFLD.
2. Materials and Methods
This is a quasi-experimental study with a pre-test/post-test design using a control group. The study population consists of all patients with NAFLD referred to the digestive health clinics in Qazvin province of Iran. After sending invitations, 55 volunteered to participate in the study. Of them, 40 were randomly selected and entered into the study based on the inclusion criteria and under the supervision of a physician. They were randomly divided into four groups: HIIT (n=10), LLE (n=10), HIIT+LLE (n=10) and control (n=10). LLE was administered for 8 weeks, 2 capsules per day. Each capsule contained 250 mg of LLE (Choufarm, South Korea) [
31]. Exercises were performed for 8 weeks, 3 sessions per week for 60 minutes with an intensity of 80-95% of heart rate reserve. Serum levels of AST, ALP, and ALT were measured by kits made by Pars Azmoun Company in Iran using enzymatic method before the intervention and 48 hours after the last training session and supplementation. Data analysis was performed using analysis of covariance and Tukey’s post hoc test considering the significance level at 0.05.
3. Results
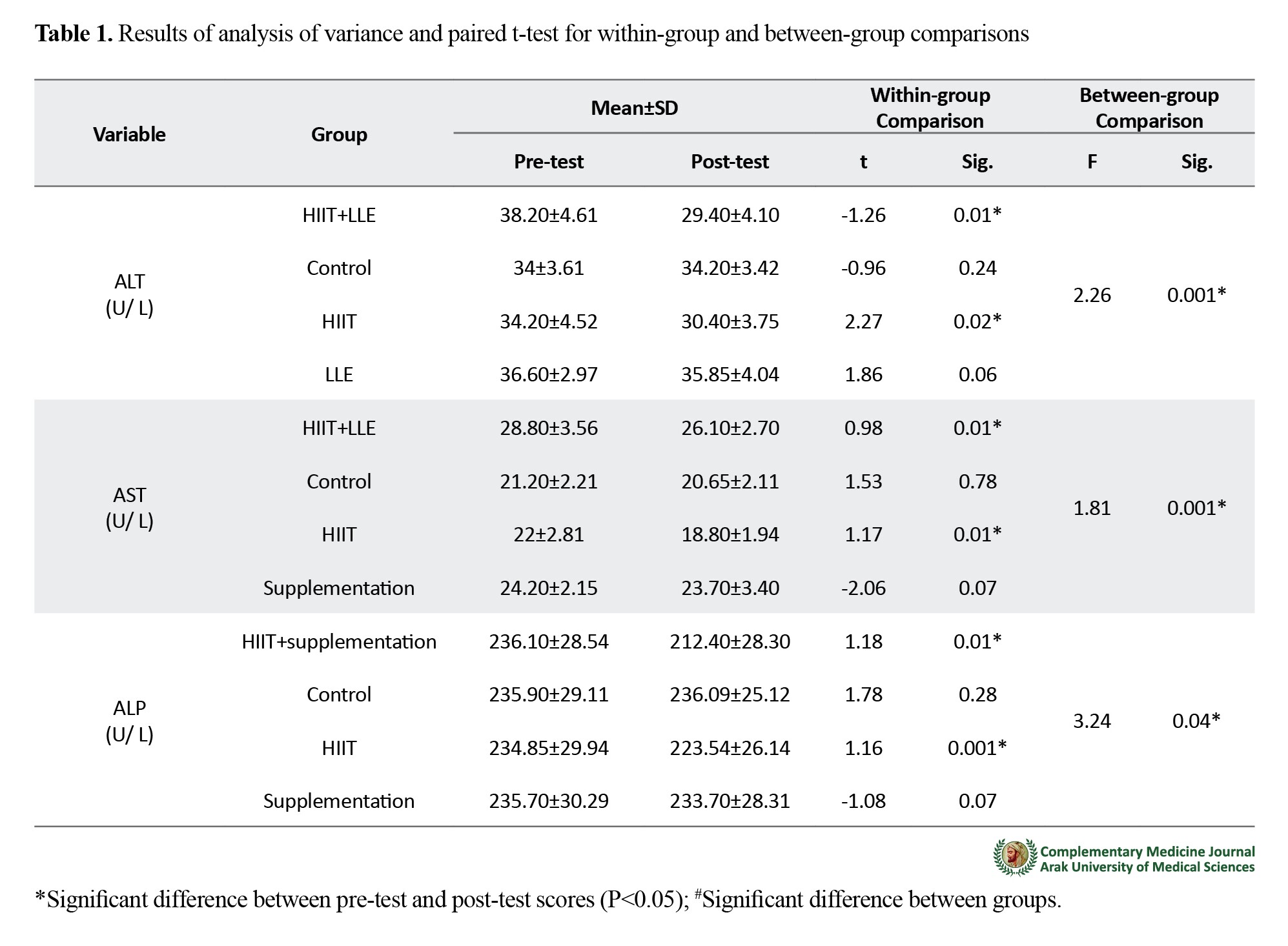
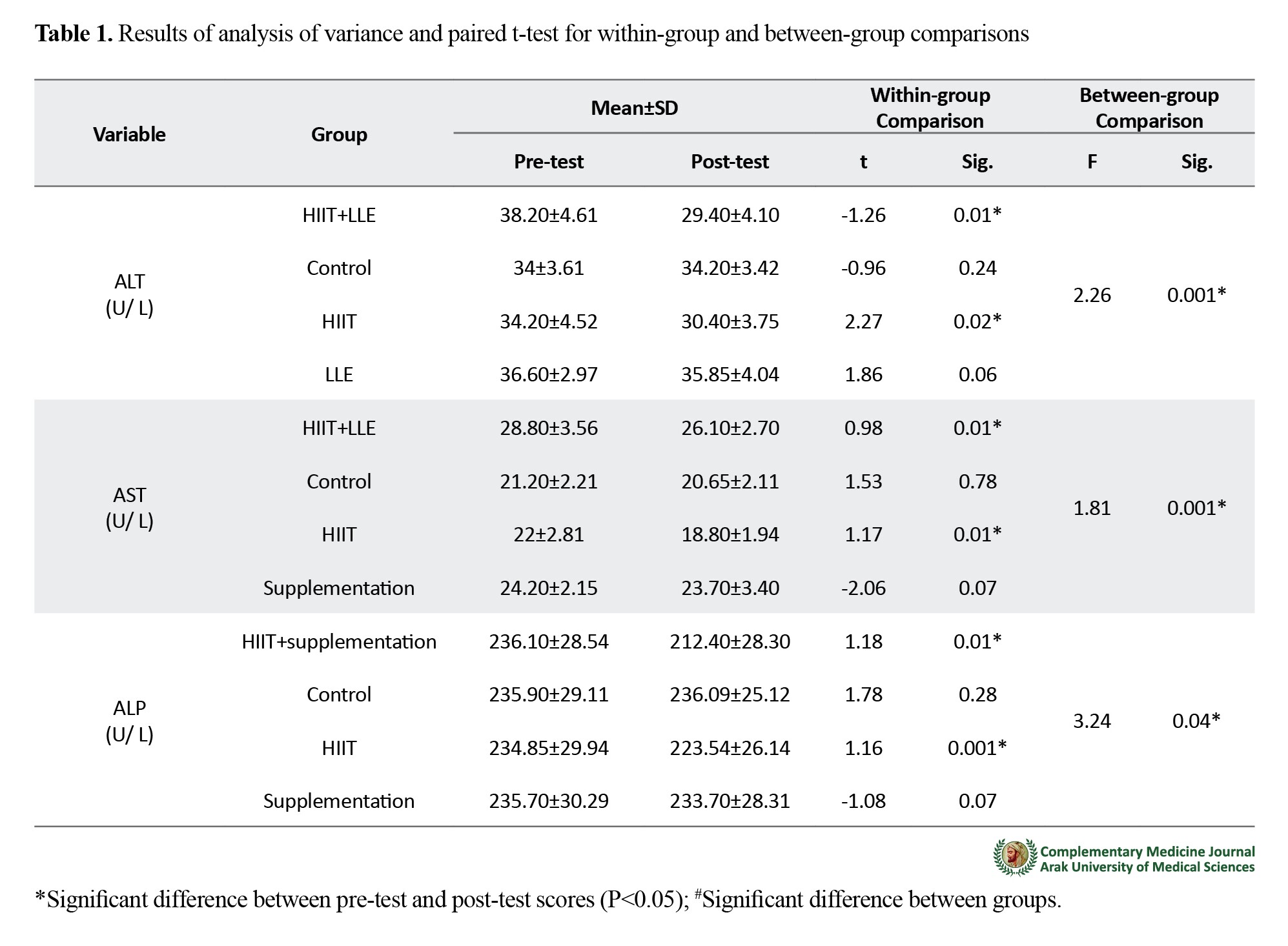
There was no significant difference between the studied groups in terms of age, weight, height, body mass index and body fat percentage (P≥0.05). The results of paired t-test showed that after eight weeks of HIIT and LLE consumption, serum ALT level significantly decreased in the HIIT+LLE (P=0.01) and HIIT (P=0.02) groups; serum AST level also significantly decreased in the in the HIIT+LLE (P=0.01) and HIIT (P=0.01) groups; serum ALP level also significantly decreased in the in the HIIT+LLE (P=0.01) and HIIT (P=0.001) groups. Analysis of covariance was used to compare the post-test scores of the groups whose results showed a significant difference between the groups in ALT (P=0.001), AST (P=0.001) and ALP (P=0.04) (
Table 1).
4. Conclusion
The results of this study regarding the effects of interval training are consistent with the results of Galedari etal [
33] and Najafi et al. [
34] but against the results of Saji et al. [
37], Fealy et al. [
38] and Hallsworth et al. [
39]. This discrepancy may be due to difference in the duration, type, and intensity of training. In Saji et al’s study, only resistance training was used while in Fealy et al’s study, endurance training was in NAFLD patients [
37,
38]. HIIT increases lipid oxidation, insulin sensitivity, and basal metabolic rate; therefore, it is possible that decreased levels of ALT (long half-life with the highest amount in liver tissue) and AST (shorter half-life) reduces liver enzymes by increasing basal metabolic rate and increasing lipid oxidation [
36]. Loquat also has high antioxidant properties which is highly related to the phenolics and flavonoids that can be found in this plant [
40]. It seems that the possible effectiveness of LLE in improving liver enzymes can be related to the antioxidant properties of ursolic acid in the plant leaves. This acid inhibits lipid peroxidation of cellular membranes by having abundant antioxidant properties and neutralizing free radicals. Moreover, it exhibits anti-inflammatory activity by decreasing cellular levels of hydrogen peroxide and nitric oxide. Therefore, due to the antioxidant and anti-inflammatory properties of ursolic acid, a decrease in the activity of liver enzymes is predictable [
23]. Possible mechanisms of action of ursolic acid include a significant response with increased apoptosis in the ROS pathway, inhibition of hyperlipidemia-induced IRE1α gene activation, and JNK phosphorylation reported in the liver of db/db mice [
45]. Overall, based on the results it can be argued that simultaneous use of LLE and HIIT can be more beneficial in improving liver enzyme status than when they are used alone.
It seems that consumption of LLE along with performing HIIT leads to a decrease in the level of liver enzymes in men with NAFLD.
Ethical Considerations
Compliance with ethical guidelines
This study obtained its ethical approval from the Ethics Committee of Imam Khomeini International University (Code: IR.IKIU.REC.1398.7346).
Funding
This study was supported by the Vice Chancellor for Research of Qazvin Imam Khomeini University and Mohaghegh Ardabili.
Authors' contributions
Conceptualization, methodology, Data collection, Data analysis: Roghayeh Afroundeh, Mohammad Ebrahim Bahram, Seyed Hamed Ghiyami Taklimi; Writing – original draft: Mohammad Ebrahim Bahram, Seyed Hamed Ghiyami Taklimi, Mahsa Gholam Hosseini; Writing – review & editing: Roghayeh Afrondeh, Mohammad Ebrahim Bahram; Final approval: Roghayeh Afroundeh, Mohammad Ebrahim Bahram, Seyed Hamed Ghayami Taklimi.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
We want to thank the Vice-Chancellor for Research of Imam Khomeini International University of Qazvin and Mohaghegh Ardabili University.
References
- St George A, Bauman A, Johnston A, Farrell G, Chey T, George J. Independent effects of physical activity in patients with nonalcoholic fatty liver disease. Hepatology. 2009; 50(1):68-76. [DOI:10.1002/hep.22940] [PMID]
- Araújo AR, Rosso N, Bedogni G, Tiribelli C, Bellentani S. Global epidemiology of non-alcoholic fatty liver disease/non-alcoholic steatohepatitis: What we need in the future. Liver International. 2018; 38(Suppl 1):47-51. [DOI:10.1111/liv.13643] [PMID]
- Davoodi M, Moosavi H, Nikbakht M. [The effect of eight weeks selected aerobic exercise on liver parenchyma and liver enzymes (AST, ALT) of fat liver patients (Persian)]. Journal of Shahrekord Uuniversity of Medical Sciences. 2012; 14(1):84-90. http://78.39.35.44/article-1-1054-fa.html
- Jahani G, Firoozrai M, Matin Homaee H, Tarverdizadeh B, Azarbayjani MA, Movaseghi GR, et al. [The effect of continuous and regular exercise on erytrocyte antioxidative enzymes activity and stress oxidative in young soccer players (Persian)]. Razi Journal of Medical Sciences. 2010; 17(74):22-32. https://www.sid.ir/en/Journal/ViewPaper.aspx?ID=186038
- Keating SE, Hackett DA, George J, Johnson NA. Exercise and non-alcoholic fatty liver disease: A systematic review and meta-analysis. Journal of Hepatology. 2012; 57(1):157-66. [DOI:10.1016/j.jhep.2012.02.023] [PMID]
- ZHOU CH, Li X, XU CJ, SUN CD, CHEN KS. Hydrophilic and lipophilic antioxidant activity of loqUAt fruits. Journal of Food Biochemistry. 2012; 36(5):621-6. [DOI:10.1111/j.1745-4514.2011.00574.x]
- Banno N, Akihisa T, Tokuda H, Yasukawa K, Taguchi Y, Akazawa H, et al. Anti-inflammatory and antitumor-promoting effects of the triterpene acids from the leaves of Eriobotrya japonica. Biological & Pharmaceutical Bulletin. 2005; 28(10):1995-9. [DOI:10.1248/bpb.28.1995] [PMID]
- Shih CC, Lin CH, Wu JB. Eriobotrya japonica improves hyperlipidemia and reverses insulin resistance in high-fat-fed mice. Phytotherapy Research. 2010; 24(12):1769-80. [DOI:10.1002/ptr.3143] [PMID]
- Ito H, Kobayashi E, Takamatsu Y, Li SH, Hatano T, Sakagami H, et al. Polyphenols from Eriobotrya japonica and their cytotoxicity against human oral tumor cell lines. Chemical & Pharmaceutical bulletin. 2000; 48(5):687-93. [DOI:10.1248/cpb.48.687] [PMID]
- Alshaker HA, Qinna NA, Qadan F, Bustami M, Matalka KZ. Eriobotrya japonica hydrophilic extract modulates cytokines in normal tissues, in the tumor of Meth-A-fibrosarcoma bearing mice, and enhances their survival time. BMC Complementary and Alternative Medicine. 2011; 11:9. [DOI:10.1186/1472-6882-11-9] [PMID] [PMCID]
- Bae D, You Y, Yoon HG, Kim K, Lee YH, Kim Y, et al. Protective effects of loqUAt (Eriobotrya japonica) leaves against ethanol-induced toxicity in HepG2 cells transfected with CYP2E1. Food Science and Biotechnology. 2010; 19(4):1093-6. [DOI:10.1007/s10068-010-0154-3]
- Kitani K, Kanai S, Ivy GO, Carrillo MC. Pharmacological modifications of endogenous antioxidant enzymes with special reference to the effects of deprenyl: A possible antioxidant strategy. Mechanisms of Ageing and Development. 1999; 111(2-3):211-21. [DOI:10.1016/S0047-6374(99)00065-2]
- Ikeda Y, Murakami A, Ohigashi H. Ursolic acid: An anti-and pro-inflammatory triterpenoid. Molecular Nutrition & Food Research. 2008; 52(1):26-42. [DOI:10.1002/mnfr.200700389] [PMID]
- Azevedo MF, Camsari C, Sá CM, Lima CF, Fernandes-Ferreira M, Pereira-Wilson C. Ursolic acid and luteolin-7-glucoside improve lipid profiles and increase liver glycogen content through glycogen synthase kinase-3. Phytotherapy Research. 2010; 24(Suppl 2):S220-4. [DOI:10.1002/ptr.3118] [PMID]
- Li S, Liao X, Meng F, Wang Y, Sun Z, Guo F, et al. Therapeutic role of ursolic acid on ameliorating hepatic steatosis and improving metabolic disorders in high-fat diet-induced non-alcoholic fatty liver disease rats. PLoS One. 2014; 9(1):e86724. [DOI:10.1371/journal.pone.0086724] [PMID] [PMCID]
- Zhao JQ, Wen YF, Bhadauria M, Nirala SK, Sharma A, Shrivastava S, et al. Protective effects of propolis on inorganic mercury induced oxidative stress in mice. New Delhi: CSIR; 2009. http://nopr.niscair.res.in/handle/123456789/3859
- Bhadauria M. Propolis prevents hepatorenal injury induced by chronic exposure to carbon tetrachloride. Evidence-based Complementary and Alternative Medicine. 2012; 2012:235358. [DOI:10.1155/2012/235358] [PMID] [PMCID]
- Saravanan R, Viswanathan P, Pugalendi KV. Protective effect of ursolic acid on ethanol-mediated experimental liver damage in rats. Life Sciences. 2006; 78(7):713-8. [DOI:10.1016/j.lfs.2005.05.060] [PMID]
- Gharibi S, Bakhtiari N, Elham-Moslemee-Jalalvand, Bakhtiari F. Ursolic acid mediates hepatic protection through enhancing of anti-aging biomarkers. Current Aging Science. 2018; 11(1):16-23. [PMID]
- Kunkel SD, Elmore CJ, Bongers KS, Ebert SM, Fox DK, Dyle MC, et al. Ursolic acid increases skeletal muscle and brown fat and decreases diet-induced obesity, glucose intolerance and fatty liver disease. PloS One. 2012; 7(6):e39332. [DOI:10.1371/journal.pone.0039332] [PMID] [PMCID]
- Moosavi-Sohroforouzani A, Ganbarzadeh M. [Reviewing the physiological effects of aerobic and resistance training on insulin resistance and some biomarkers in non-alcoholic fatty liver disease (Persian)]. Feyz Journal of Kashan University of Medical Sciences. 2016; 20(3):282-96. http://feyz.kaums.ac.ir/article-1-3091-en.html
- Pingitore A, Lima GP, Mastorci F, Quinones A, Iervasi G, Vassalle C. Exercise and oxidative stress: Potential effects of antioxidant dietary strategies in sports. Nutrition. 2015; 31(7-8):916-22. [DOI:10.1016/j.nut.2015.02.005] [PMID]
- Slentz CA, Bateman LA, Willis LH, Shields AT, Tanner CJ, Piner LW, et al. Effects of aerobic vs. resistance training on visceral and liver fat stores, liver enzymes, and insulin resistance by HOMA in overweight adults from STRRIDE AT/RT. American Journal of Physiology-Endocrinology and Metabolism. 2011; 301(5):E1033-9. [DOI:10.1152/ajpendo.00291.2011] [PMID] [PMCID]
- Shamsoddini A, Sobhani V, Ghamar Chehreh ME, Alavian SM, Zaree A. Effect of aerobic and resistance exercise training on liver enzymes and hepatic fat in Iranian men with nonalcoholic fatty liver disease. Hepatitis Monthly. 2015; 15(10):e31434. [DOI:10.5812/hepatmon.31434] [PMID] [PMCID]
- Barani F, Afzalpour M E, Ilbiegi S, Kazemi T, Mohammadi Fard M. [The effect of resistance and combined exercise on serum levels of liver enzymes and fitness indicators in women with nonalcoholic fatty liver disease (Persian)]. Journal of Birjand University of Medical Sciences. 2014; 21(2):188-202. http://journal.bums.ac.ir/article-1-1588-en.html
- Behzadimoghadam M, Galedari M, Motalebi L. [The effect of eight weeks resistance training and low-calorie diet on plasma levels of liver enzymes and liver fat in Non-Alcoholic Fatty Liver Disease (NAFLD) (Persian)]. Iranian Journal of Nutrition Sciences & Food Technology. 2018; 12(4):25-32. http://nsft.sbmu.ac.ir/article-1-2356-en.html
- Alie M, Matinhomaee H, Azarbayjani MA, Piri M. [The effect of different resistance training intensities on liver function in obese men (Persian)]. Journal of Sport Biosciences. 2017; 9(1):75-92. [DOI:10.5812/hepatmon.31434]
- Kistler KD, Brunt EM, Clark JM, Diehl AM, Sallis JF, Schwimmer JB; NASH CRN Research Group. Physical activity recommendations, exercise intensity, and histological severity of nonalcoholic fatty liver disease. The American Journal of Gastroenterology. 2011; 106(3):460-8. [DOI:10.1038/ajg.2010.488] [PMID] [PMCID]
- Tondpa Khaghani B, Dehkhoda M R, Amani Shalamzari S. [Improvement of aerobic power and health status in overweight patients with non-alcoholic fatty liver disease with high intensity interval training (Persian)]. Journal of Payavard Salamat. 2019; 13(1):71-80. http://payavard.tums.ac.ir/article-1-6700-en.html
- Hood MS, Little JP, Tarnopolsky MA, Myslik F, Gibala MJ. Low-volume interval training improves muscle oxidative capacity in sedentary adults. Medicine and Science in Sports and Exercise. 2011; 43(10):1849-56. [DOI:10.1249/MSS.0b013e3182199834] [PMID]
- Cho YH, Lee SY, Kim CM, Kim ND, Choe S, Lee CH, et al. Effect of loquat leaf extract on muscle strength, muscle mass, and muscle function in healthy adults: A randomized, double-blinded, and placebo-controlled trial. Evidence-Based Complementary and Alternative Medicine. 2016; 2016:4301621. [DOI:10.1155/2016/4301621] [PMID] [PMCID]
- Esfahani FH, Asghari G, Mirmiran P, Azizi F. Reproducibility and relative validity of food group intake in a food frequency questionnaire developed for the Tehran Lipid and Glucose Study. Journal of Epidemiology. 2010; 20(2):150-8. [DOI:10.2188/jea.JE20090083] [PMID] [PMCID]
- Galedari M, Kaki A. [The effect of 12 weeks high intensity interval training and resistance training on liver fat, liver enzymes and insulin resistance in men with nonalcoholic fatty liver (Persian)]. Jundishapur Scientific Medical Journal. 2017;16(5):493-503. [DOI:10.2188/jea.JE20090083]
- Najafi L, Azizi M, Tahmasebi V. [The effect of 6 weeks HIIT training in the conditions of hypoxia and normoxia on liver enzymes levels and lipid profiles in overweight women (Persian)]. Journal of Applied Health Studies in Sport Physiology. 2016; 3(2):56-63. [DOI:10.2188/jea.JE20090083]
- Moradi Kelardeh B, Azarbayjani MA, Peeri M, Homaee HM. [Effects of nonlinear resistance training on liver biochemical marker levels in postmenopausal women with nonalcoholic fatty liver disease (Persian)]. Scientific Journal of Rehabilitation Medicine. 2017; 5(4):136-45. [DOI:10.2188/jea.JE20090083]
- Skrypnik D, Ratajczak M, Karolkiewicz J, Mądry E, Pupek-Musialik D, Hansdorfer-Korzon R, et al. Effects of endurance and endurance-strength exercise on biochemical parameters of liver function in women with abdominal obesity. Biomedicine & Pharmacotherapy. 2016; 80:1-7. [DOI:10.1016/j.biopha.2016.02.017] [PMID]
- Zelber-Sagi S, Ratziu V, Oren R. Nutrition and physical activity in NAFLD: An overview of the epidemiological evidence. World Journal of Gastroenterology. 2011; 17(29):3377-89. [DOI:10.3748/wjg.v17.i29.3377] [PMID] [PMCID]
- Fealy CE, Haus JM, Solomon TP, Pagadala M, Flask CA, McCullough AJ, et al. Short-term exercise reduces markers of hepatocyte apoptosis in nonalcoholic fatty liver disease. Journal of Applied Physiology. 2012; 113(1):1-6. [DOI:10.1152/japplphysiol.00127.2012] [PMID] [PMCID]
- Hallsworth K, Fattakhova G, Hollingsworth KG, Thoma C, Moore S, Taylor R, et al. Resistance exercise reduces liver fat and its mediators in non-alcoholic fatty liver disease independent of weight loss. Gut. 2011; 60(9):1278-83. [DOI:10.1136/gut.2011.242073] [PMID] [PMCID]
- Zhou C, Sun C, Chen K, Li X. Flavonoids, phenolics, and antioxidant capacity in the flower of Eriobotrya japonica Lindl. International Journal of Molecular Sciences. 2011; 12(5):2935-45. [DOI:10.3390/ijms12052935] [PMID] [PMCID]
- YYoshioka S, Hamada A, Jobu K, Yokota J, Onogawa M, Kyotani S, et al. Effects of Eriobotrya japonica seed extract on oxidative stress in rats with non-alcoholic steatohepatitis. Journal of Pharmacy and Pharmacology. 2010; 62(2):241-6. [DOI:10.1211/jpp.62.02.0012] [PMID]
- Shahat AA, Ullah R, Alqahtani AS, Alsaid MS, Husseiny HA, Al Meanazel OTR. Hepatoprotective effect oferiobotrya japonica leaf extract and its various fractions against carbon tetra chloride induced hepatotoxicity in rats. Evidence-Based Complementary and Alternative Medicine. 2018, 2018:3782768. [DOI:10.1155/2018/3782768] [PMID] [PMCID]
- Mun J, Park J, Yoon HG, You Y, Choi KC, Lee YH, et al. Effects of eriobotrya japonica water extract on alcoholic and nonalcoholic fatty liver impairment. Journal of Medicinal Food. 2019; 22(12):1262-70. [DOI:10.1089/jmf.2019.4493] [PMID]
- Nishioka Y, Yoshioka S, Kusunose M, Cui T, Hamada A, Ono M, et al. Effects of extract derived from Eriobotrya japonica on liver function improvement in rats. Biological & Pharmaceutical Bulletin. 2002; 25(8):1053-7. [DOI:10.1248/bpb.25.1053] [PMID]
- Li JS, Wang WJ, Sun Y, Zhang YH, Zheng L. Ursolic acid inhibits the development of nonalcoholic fatty liver disease by attenuating endoplasmic reticulum stress. Food & Function. 2015; 6(5):1643-51. [DOI:10.1039/C5FO00083A] [PMID]


 , Roghayeh Afroundeh1
, Roghayeh Afroundeh1 

 , Seyed Hamed Ghiyami Taklimi
, Seyed Hamed Ghiyami Taklimi 

 2, Abbas Sadeghi3
2, Abbas Sadeghi3 

 , Mahsa Gholamhosseini3
, Mahsa Gholamhosseini3