1. Introduction
troke is one of the leading causes of long-term disability in adults. Stroke damages the sensory, motor, perceptual, visual, and cognitive systems, impairing the patient’s ability to perform daily activities of life. About 30%-40% of people who survive a stroke have severe disabilities that reduce their functional abilities, including the ability to walk. Given that impaired balance and walking and a high risk of falling at all stages after a stroke have been reported as a major problem in stroke patients, improving balance and gait with proper speed and safety is the main goal in rehabilitation of people with stroke. One of the new methods of treating stroke patients is mirror therapy. This method focuses on the movements of the limbs with no injury; during the mirror therapy, the person pays attention to the movements of healthy limbs in the mirror and receives visual feedback. Mirror therapy is an affordable and easy method that does not require a lot of energy and patients can continue the treatment themselves after learning how to perform the movements, and is as an alternative to costly complementary therapies after stroke. Mirror therapy can increase neuroplasticity (adaptation of nerve cells) in the brain by creating appropriate sensory inputs, and is an alternative to the lack or reduced proprioception in the affected side of the body. The aim of this study is to answer the question that mirror therapy in which subacute and chronic stages after stroke has a greater effect on patients’ walking rehabilitation?
2. Materials and Methods
This is a quasi-experimental study with pre-test/post-test design. The study population consists of all patients with stroke referred to Tabassom Clinic in Tehran, Iran (n=150). The sample size was estimated 30 according to the previous studies and the formula. Samples were 15 patients with subacute stage and 15 patients with chronic stage after stroke undergoing physiotherapy, who met the inclusion criteria and were selected using a purposive sampling method. First, the purpose and method of study was explained to each patient and then a written informed consent was obtained from them. Finally, by excluding 2 patients in the chronic group and 5 patients in the subacute group, this study was performed with 23 samples. The instruments used in this study included a demographic form and the Gait Assessment and Intervention Tool (GAIT). The demographic form had 9 questions that were completed using the patients’ medical records and interview with them. The GAIT consisted of 31 motor functions that are divided into 3 sections related to three phases of the gait cycle. The reliability of this test has been confirmed by calculating the internal consistency and inter-rater reliability and its validity has been confirmed by simultaneous evaluation with other scales. The gait of all patients was filmed in three directions: anterior, posterior and lateral; and scoring was done according to the GAIT instructions by reviewing the recorded videos. The GAIT was performed in both subacute and chronic groups before and after the intervention.
Both groups have had their interventional program for 8 weeks, 2 sessions per week for a 1.5 hours (total= 16 sessions). It consisted of 60 minutes of routine rehabilitation (nerve relaxation techniques, muscle tone adjustment exercise, muscle strength exercise, walking exercise, and weight transfer exercise), and 30 minutes of mirror therapy at 16 sessions, one session per day, in two separate parts: mirror therapy exercises and balance exercises with a mirror, each for 15 minutes. The patient did not receive any verbal feedback during mirror therapy. The difference between the experimental and control groups was only in the use of the mirror during the exercises. Data were analyzed using independent t-test and ANCOVA in SPSS version 23 software considering a significance level of 0.05.
3. Results
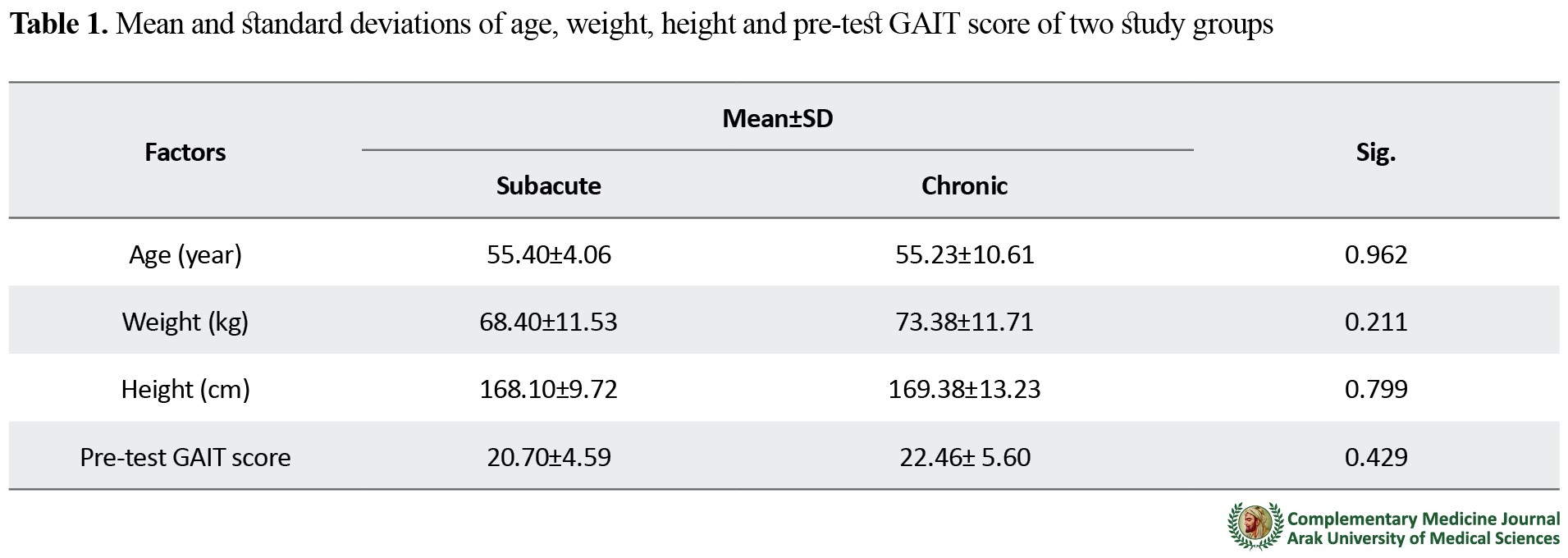
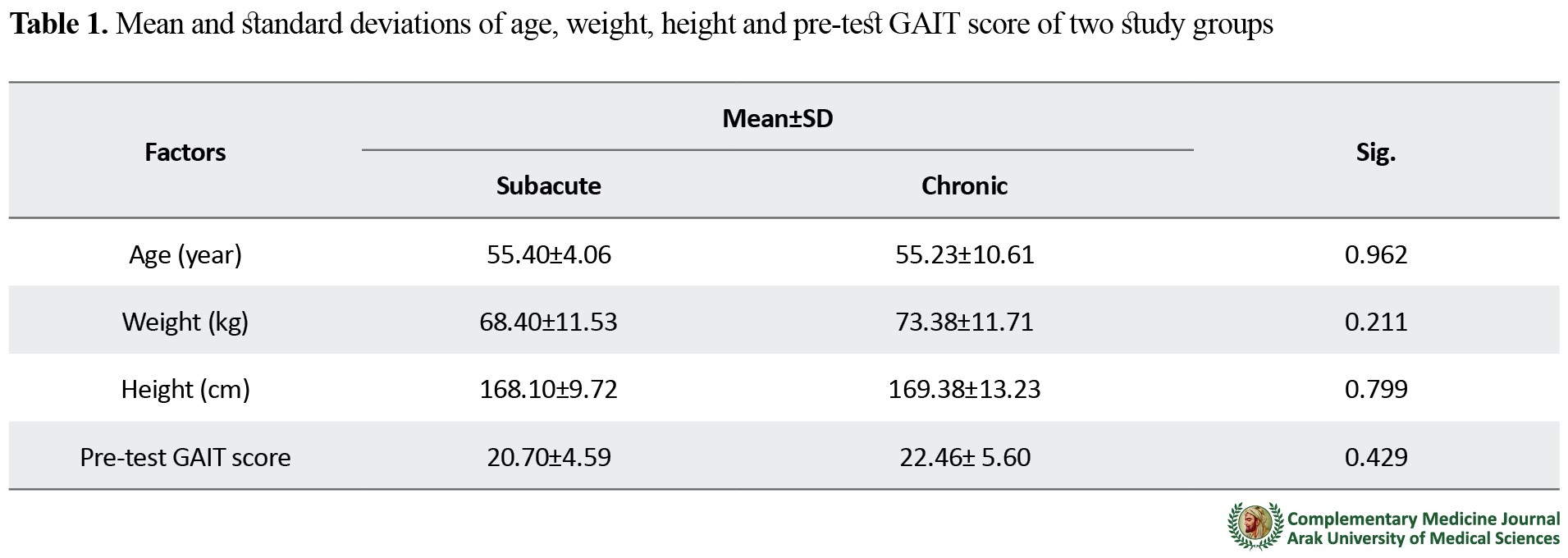
Mean and standard deviations of age, weight, height and GAIT score of two study groups and the results of comparison between the two groups using independent t-test are reported in
Table 1.
Dependent t-test was used to evaluate the difference between pre-test and post-test scores in the two groups separately. The results showed a significant difference between pre-test and post-test scores in each group (
Table 2).

To compare the results of GAIT-test in both groups in the post-test phase, considering the pre-test score as a covariate factor, the ANCOVA was used. The results showed a significant difference in the post-test GAIT score of two groups. The results also showed that the pre-test GAIT score had a significant effect on its post-test score (
Table 3).
 4. Conclusion
4. Conclusion
Mirror therapy is useful for walking rehabilitation of patients with subacute and chronic stroke, but in the subacute stage it has completely better results. Therefore, it is recommended to use mirror therapy to rehabilitate the walking of stroke patients at subacute phase.
Ethical Considerations
Compliance with ethical guidelines
This article has an ethical approval from the Research Ethics Committee of Sport Sciences Research Institute of Iran (Code: IR.SSRI.REC.1399.751).
Funding
The present paper was extracted from the MSc. thesis of the first author, Department of Physical Education and Sports Sciences, Faculty of Literature and Humanities, University of Shahrekord.
Authors' contributions
Conceptualization, methodology: All authors; Investigation, writing – original draft: Shima Shahidi, Ali Shafizadeh; Writing – review & editing, resources: Ali Shafizadeh; Supervision: Ali Shafizadeh
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
The authors would like to thank the head of Tabassom Clinic and all patients for their valuable cooperation.
References
- World Health Organization. The global health observatory [Internet]. 2010 [Retrieved: 2015 November 20]. Availebale from: https://www.who.int/data/gho
- Salman-Roghani R, Delbari A, Tabatabae S S. [Stroke rehabilitation: Principles, advances, early experiences, and realities in Iran (Persian)]. Journal of Sabzevar University of Medical Sciences. 2012; 19(2):96-107. https://www.sid.ir/en/journal/ViewPaper.aspx?id=266467
- Sahebalzamani M, Alilou L, Shakibi A. The efficacy of self-care education on rehabilitation of stroke patients. Saudi Medical Journal. 2009; 30(4):550-4. https://www.semanticscholar.org/paper/
- Akbari A, Karimi H, Kazemnegad A, Ghabaii M. [The effect of strengthening exercises on biomechanical parameters of gait in chronic hemi paresis following stroke (Persian)]. Journal of Inflammatory Diseases. 2005; 9(3):8-15. http://journal.qums.ac.ir/article-1-718-en.html
- World Health Organization. Global status report on noncommunicable diseases [Internet]. 2014. [Retrieved: 2015 November 15]. Availabale from http://www.who.int/nmh/publications/ncd-status-report- 2014/en/
- American Heart Association. Heart disease and stroke statistics. Dallas: TX American Heart Association. 2005.
- Beyaertab C, Vasac R, Frykberg GE. Gait post-stroke: Pathophysiology and rehabilitation strategies. Neurophysiologie Clinique/Clinical Neurophysiology. 2015; 45(4):335-355. [DOI:10.1016/j.neucli.2015.09.005] [PMID]
- Kim MK, Ji SG, Cha HG. The effect of mirror therapy on balance ability of subacute stroke patients. Hong Kong Physiotherapy Journal. 2016; 34:27-32. [DOI:10.1016/j.hkpj.2015.12.001] [PMID] [PMCID]
- Sütbeyaz S, Yavuzer G, Sezer N, Koseoglu F. Mirror therapy enhances lower-extremity motor recovery and motor functioning after stroke: A randomized controlled trial. Archives of Physical Medicine and Rehabilitation. 2007; 88(5):555-9. [DOI:10.1016/j.apmr.2007.02.034] [PMID]
- Ji SG, Kim MK. The effects of mirror therapy on the gait of subacute stroke patients: A randomized controlled trial. Clinical Rehabilitation. 2015; 29(4):348-54. [DOI:10.1177/0269215514542356] [PMID]
- Stubbs PW, Nielsen JF, Sinkjær T, Mrachacz-Kersting N. Short-latency crossed spinal responses are impaired differently in sub-acute and chronic stroke patients. Clinical Neurophysiology. 2012; 123(3):541-549. [DOI:10.1016/j.clinph.2011.07.033] [PMID]
- Abo-Salem HM, Xiaolin H. The effects of mirror therapy on clinical improvement in hemiplegic lower extremity rehabilitation in subjects with chronic stroke. World Academy of Science, Engineering and Technology, International Journal of Medical, Health, Biomedical, Bioengineering and Pharmaceutical Engineering. 2015; 9(2):163-6. [DOI.10.5281/zenodo.1099406]
- Cha HG, kim MK. The effects of repetitive transcranial magnetic stimulation integrated mirror therapy on the gait of chronic stroke patients. Journal of Magnetics. 2015; 20(2):133-7. [DOI:10.4283/JMAG.2015.20.2.133]
- Cho KH, Lee WH. Effect of treadmill training based real-world video recording on balance and gait in chronic stroke patients: A randomized controlled trial. Gait & Posture. 2014; 39(1):523-528. [DOI:10.1016/j.gaitpost.2013.09.003] [PMID]
- Lee Y, Lin K, Wu C, Liao C, Lin J, Chen C. Combining afferent stimulation and mirror therapy for improving muscular, sensorimotor and daily functions after chronic stroke: A randomized, placebo-controlled study. American Journal of Physical Medicine & Rehabilitation. 2015; 94(10S):859- 68. [DOI:10.1097/PHM.0000000000000271] [PMID]
- Srivastava A, Taly AB, Guptab A, Kumarb S, Muralid T. Bodyweight-supported treadmill training for retraining gait among chronic stroke survivors: A randomized controlled study. Annals of Physical and Rehabilitation Medicine. 2016; 59(4):235-41. [DOI:10.1016/j.rehab.2016.01.014] [PMID]
- Arya KN. Underlying neural mechanisms of mirror therapy: Implications for motor rehabilitation in stroke. Neurology India. 2016; 64(1):38. [DOI:10.4103/0028-3886.173622] [PMID]
- Sathian K, Greenspan A I, Wolf S L. Doing it with mirrors: A case study of a novel approach to neurorehabilitation. Neurorehabilitation and Neural Repair. 2000; 14(1): 73-76. [DOI:10.1177/154596830001400109] [PMID]
- Flor H, Diers M. Sensorimotor training and cortical reorganization. Neuro Rehabilitation. 2009; 25(1):19-27. [DOI:10.3233/NRE-2009-0496] [PMID]
- Lee HJ, Kim Y M, Lee DK. The effects of action observation training and mirror therapy on gait and balance in stroke patients. Journal of Physical Therapy Science. 2017; 29(3):523-526. [DOI:10.1589/jpts.29.523] [PMID] [PMCID]
- Arya KN, Pandian S, Kumar V. Effect of activity-based mirror therapy on lower limb motor-recovery and gait in stroke: A randomised controlled trial. Neuropsychological Rehabilitation. 2019; 29(8):1193-210. [DOI:10.1080/09602011.2017.1377087] [PMID]
- Wu CY, Huang PC, Chen YT, Lin KC, Yang HW. Effects of mirror therapy on motor and sensory recovery in chronic stroke: a randomized control trial. Archives of Physical Medicine and Rehabilitation. 2013; 94:1023-30. [DOI:10.1016/j.apmr.2013.02.007] [PMID]
- Hung GK N, Li CT L, Yiu AM, Fong KNK. Systematic review: Effectiveness of mirror therapy for lower extremity post-stroke. Hong Kong Journal of Occupational Therapy. 2015; 26:51-59. [DOI:10.1016/j.hkjot.2015.12.003]
- Chopra C, Tamaria S. Mirror Therapy in Stroke Rehabilitation. International Journal of Science and Research. 2015; 4(7):660-663. https://www.researchgate.net/publication/334389428
- Rahimi G, Zamani A. Introduction to research method in physical education.1st ed, Isfahan. Khorasgan: Azad University of Isfahan Branch Khorasgan; 2009.
- Daly JJ. Nethery J, McCabe JP, Brenner I, Rogers J, Gansen J, et al. Development and testing of the Gait Assessment and Intervention Tool (GAIT): A measure of coordinated gait components. Journal of Neuroscience Methods. 2009; 178(2):334-339. [DOI:10.1016/j.jneumeth.2008.12.016] [PMID]
- Zimbelman J, Daly JJ, Roenigk KL, Butler K, Burdsall R, Holcomb JP. Capability of 2 gait measures for detecting response to gait training in stroke survivors: Gait Assessment and Intervention Tool and the Tinetti Gait Scale. Archives of Physical Medicine and Rehabilitation. 2012; 93(1):129-36. [DOI:10.1016/j.apmr.2011.08.011] [PMID]
- Ferrarello F, Bianchi VA, Baccini M, Rubbieri G, Mossello E, Cavallini MC et al. Tools for observational gait analysis in patients with stroke: A systematic review. Physical Therapy. 2013;93(12):1673-85. [DOI:10.2522/ptj.20120344] [PMID]
- Gor-García-Fogeda MD, Cano de la Cuerda R, Carratalá Tejada M, Alguacil-Diego IM, Molina-Rueda F. Observational gait assessments in people with neurological disorders: A systematic review. Archives of Physical Medicine and Rehabilitation. 2015; 97(1):131-40. [DOI:10.1016/j.apmr.2015.07.018] [PMID]
- Hamdy S, Rothwell J C, Aziz Q, Singh KD, Thompson DG. Long-term reorganization of human motor cortex driven by shortterm sensory stimulation. Nature Neuroscience. 1998; 1(1):64-8. [DOI:10.1038/264] [PMID]
- Toh SF, Fong KN. Systematic review on the effectiveness of mirror therapy in training upper limb hemiparesis after stroke. Hong Kong Journal of Occupational Therapy. 2012; 22(2):84-95. [DOI:10.1016/j.hkjot.2012.12.009]
- Holmes NP, Crozier G, Spence C. When mirrors lie: “Visual capture” of arm position impairs reaching performance. Cognitive, Affective, & Behavioral Neuroscience. 2004; 4:193-200 [DOI:10.3758/CABN.4.2.193] [PMID] [PMCID]
- Reynolds JE, Licari MK, Billington J, Chen Y, Aziz-Zadeh L, Werner J, et al. Mirror neuron activation in children with developmental coordination disorder: A functional MRI study. International Journal of Developmental Neuroscience. 2015; 47:309-319. [DOI:10.1016/j.ijdevneu.2015.10.003] [PMID]
- Mattys K, Smits M, Van der Geest JN, Van der Lugt A, Seurinck R, Stam HJ, et al. Mirror induced visual illusion of hand movements: a functional magnetic resonance imaging study. Archives of Physical Medicine and Rehabilitation. 2009; 90:675-81. [DOI:10.1016/j.apmr.2008.09.571] [PMID]
- Ramachandran VS, Rogers Ramachandran D. Synaesthesia in phantom limbs induced with mirrors. Proceedings of the royal society B. Biological Sciences. 1996; 263:377-86. [DOI:10.1098/rspb.1996.0058] [PMID]
- Shih TY, Wu CY, Lin KC, Cheng CH, Hsieh YW, Chen CL, et al. Effects of action observation therapy and mirror therapy after stroke on rehabilitation outcomes and neural mechanisms by MEG: Study protocol for a randomized controlled trial. Trials. 2017; 18(1):459. [DOI:10.1186/s13063-017-2205-z] [PMID] [PMCID]
- Mazlom SR, Bahrami M, Hasanzadeh F, Ghandehari K. [Effect of mirror therapy on walking ability in patients with stroke (Persian)]. Journal of Birjand University of Medical Sciences. 2015; 22 (2):134-144. http://journal.bums.ac.ir/article-1-1765-en.html
- Shabaani Mehr M, Khaleghdoost Mohammadi T, Jafroudi S, Kazemnezhad Leyli E, Majd Teimoori Z. The effect of mirror therapy on the walking ability of patients after stroke. Journal of Holistic Nursing And Midwifery. 2019; 29(4):200-9. [DOI:10.32598/ JHNM.29.4.200]
- Louie DR, Lim SB, Eng JJ. The efficacy of lower extremity mirror therapy for improving balance, gait, and motor function poststroke: A systematic review and meta-analysis. Journal of Stroke and Cardiovascular Disease. 2019; 28(1):107-20. [DOI:10.1016/j.jstrokecerebrovasdis.2018.09.017] [PMID]
- Gandhi DBC, Sterba A, Khatter H, Pandian JD. Mirror therapy in stroke rehabilitation: Current perspectives. Therapeutics and Clinical Risk Management. 2020; 16:75-85. [DOI:10.2147/TCRM.S206883] [PMID] [PMCID]
- Bhoraniya SH, Mishra DG, Parikh SR. The effect of mirror therapy on the gait of chronic stroke patients: A randomized controlled trial. National Journal of Physiology, Pharmacy and Pharmacology. 2018; 8(9):1321-5. [DOI:10.5455/njppp.2018.8.0412506062018]
- Cha HG, Oh DW. Effects of mirror therapy integrated with task-oriented exercise on the balance function of patients with poststroke hemiparesis: A randomized-controlled pilot trial. International Journal of Rehabilitation Research. 2016; 39(1):70-76. [DOI:10.1097/MRR.0000000000000148] [PMID]
- Mohan U. Effectiveness of mirror therapy on lower extremity motor recovery, balance and mobility in patients with acute stroke: A randomized sham-controlled pilot trial. Annals of Indian Academy of Neurology. 2013; 16(4):634. [DOI:10.4103/0972-2327.120496] [PMID] [PMCID]
- In T, Lee K, Song C. Virtual reality reflection therapy improves balance and gait in patients with chronic stroke: Randomized controlled trials. Medical science monitor: International medical journal of Experimental and Clinical Research. 2016; 22:4046-53. [DOI:10.12659/MSM.898157] [PMID] [PMCID]